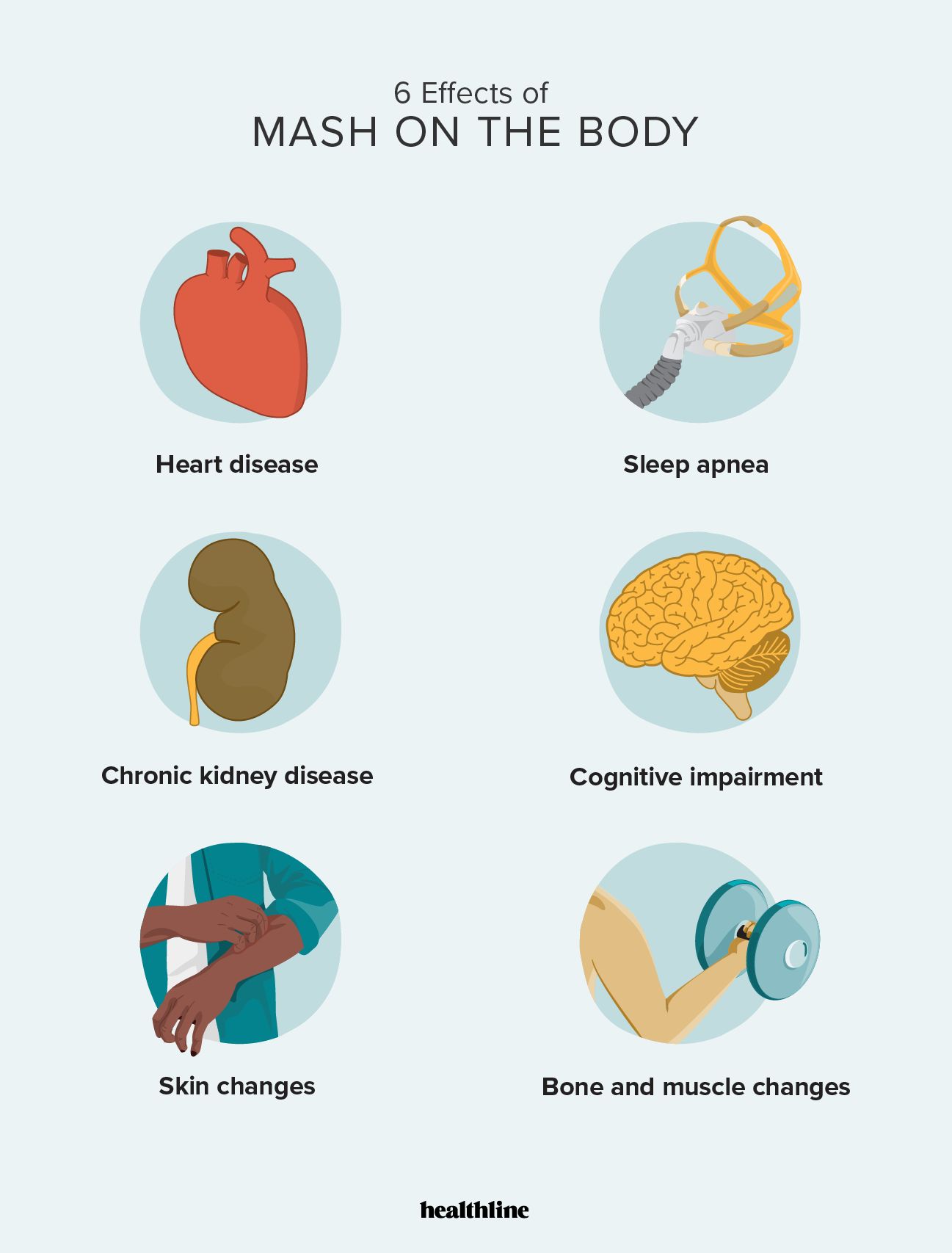
Metabolic dysfunction-associated steatohepatitis (MASH) starts in your liver, but it can have body-wide effects. These effects increase your risk of conditions like heart disease, chronic kidney disease, and cognitive impairment.
MASH is the updated term for a type of liver disease once known as nonalcoholic steatohepatitis (NASH). It’s the more serious form of metabolic dysfunction-associated steatotic liver disease (MASLD), a condition once known as nonalcoholic fatty liver disease (NAFLD).
In MASLD, dysfunction in your metabolic system causes fat to build up in your liver. At this stage, the chance of liver damage is low, and you might not notice any symptoms. If MASLD progresses and inflammation, liver cell damage, and fibrosis (scarring) also occur, MASLD becomes MASH.
Not everyone living with MASLD develops MASH. Certain factors, including obesity, metabolic syndrome, age, and genetics, can play a role in the likelihood of progression.
Because early symptoms of MASH can be absent or nonspecific, like fatigue, weight loss, or abdominal discomfort, MASH can go undetected and have major health consequences.
Extensive scarring of the liver (cirrhosis) and liver failure are serious concerns in MASH. But MASH can pose risks to the rest of your body, too.
MASLD and MASH are highly associated with an increased risk of heart disease. In fact, heart disease is the number one cause of death among people with MASLD.
Inflammation from MASH can damage blood vessels throughout the body. It can also promote the buildup of plaque, which blocks blood vessels and keeps them from dilating properly, which in turn restricts blood flow.
Dyslipidemia (altered lipid metabolism) and insulin resistance from metabolic dysfunction in MASH can also promote blood vessel damage and plaque buildup.
As blood vessels stiffen and become restricted, hypertension (high blood pressure) can develop. Other heart conditions doctors see in people with MASLD and MASH include:
- coronary artery disease
- angina (chest pain)
- ischemic stroke
- congestive heart failure
- arrhythmia (irregular heart beat)
MASH and sleep apnea share several risk factors, such as obesity, metabolic dysfunction, and chronic inflammation. Living with MASH
Body-wide inflammation from MASH can affect your airways, causing swelling that restricts your breathing while you sleep.
Insulin resistance in MASH can also promote fat buildup in areas like the neck and upper airway, increasing the likelihood of airway collapse or obstruction while sleeping.
Chronic kidney disease (CKD) refers to a gradual loss of kidney function, which leads to an excess of toxins and waste build-up in the body.
MASH can contribute to CKD by damaging blood vessels and kidney tissue through persistent inflammation, hypertension, and other imbalances, like insulin resistance, that affect the integrity of your blood vessels.
This damage can cause kidney scarring that negatively affects how your kidneys function.
Body-wide inflammation from MASH can affect your brain function. According to a review from 2021, MASH is associated with cognitive deficits such as:
- reduced memory
- impaired spatial learning
- depressive behaviors
These cognitive changes can arise from body-wide inflammation in MASH that contributes to pro-inflammatory substances in brain tissue, disruptions in the blood-brain barrier, and activation of central nervous system immune cells called microglia.
Research from 2025 notes that the risk of developing cognitive impairments appears to be four times higher among people with MASLD compared with people who don’t have the condition.
Your liver is responsible for many functions, including:
- detoxifying the body
- synthesizing proteins
- regulating blood sugar levels
When your liver function becomes severely impaired due to MASH, substances that may lead to skin symptoms can build up.
For example too much bilirubin in the body can lead to jaundice (yellowing of the skin). A buildup of bile salts in the blood stream can lead to skin itch. And excessive hormones in the blood stream can contribute to visible vascular changes, like spider angiomas.
What’s more, circulatory changes in MASH can also contribute to the appearance of spider veins and easy bruising. Insulin resistance may contribute to skin discoloration. And chronic inflammation can promote rashes or dermatitis.
Sarcopenia (muscle wasting and weakness) can occur in MASH due to chronic inflammation, which accelerates muscle breakdown, and from fatty deposits accumulating in muscle tissue, which disrupts muscle function.
Your bone health can also become compromised in MASH. Liver dysfunction prevents bone-related nutrient absorption, restricts protein production, and causes lipotoxicity (fat toxicity), all of which can negatively affect bone mineralization.
MASH is the progressive form of MASLD. Understanding your personal risk factors for developing MASLD and MASH can help you take steps to become proactive about prevention. Knowing your risk level can also support people getting a diagnosis as soon as possible.
For many people, early diagnosis and treatment can prevent MASLD from becoming MASH. And if you receive a diagnosis of MASH, treatment can help slow or reverse damage to your liver in some cases.
It’s best to speak with a doctor about MASLD and MASH if you have any of the following risk factors:
- obesity
- insulin resistance
- type 2 diabetes
- dyslipidemia (altered lipid metabolism)
- hypertension (high blood pressure)
- metabolic syndrome
- advanced age
- a known genetic susceptibility (for example, if you have the PNPLA3, TM6SF2, or MBOA7 genes)
- a sedentary lifestyle
- a diet high in saturated fats, refined sugars, and processed foods
- Hispanic ancestry (Hispanic adults are 1.42 times as likely to develop MASH compared with non-Hispanic adults)
Treatment of MASH typically involves lifestyle strategies such as diet and exercise, as well as targeted weight loss. Losing a total of 10% of your body weight can help reduce fat and inflammation in MASH and may reverse the early stages of liver scarring.
In 2024, the
Other promising drugs for MASH in the clinical trial phase include:
- semaglutide
- survodutide
- tirzepatide
If you have any health conditions known to co-exist with MASH, like sleep apnea, your doctor will also create a treatment plan that addresses those health concerns alongside MASH management.
In severe cases, where damage to the liver is significant and liver function can’t support the body’s needs, a liver transplant may be necessary.
Metabolic dysfunction-associated steatohepatitis (MASH) is an advanced form of liver disease caused by inflammation, tissue damage, and the build-up of fatty deposits in your liver. While cirrhosis and liver failure are serious concerns with this condition, MASH can also affect various parts of your body other than the liver.
Without treatment, MASH can lead to complications from insulin resistance, dyslipidemia, chronic inflammation, and other disrupted bodily processes, which can contribute to conditions like heart disease, kidney disease, and cognitive impairment.
Understanding your risk of developing MASH can help you focus on prevention and early treatment. Some people may be able to reverse many effects of MASH when doctors detect it early.